High hip survival rate seen after hip arthroscopy in patients with dysplastic hips
Source: Healio
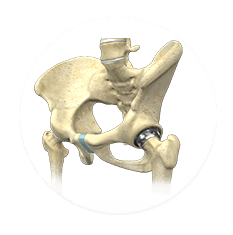
Seventy percent of patients with hip dysplasia who underwent hip arthroscopy did not require total hip arthroplasty at 5 years and demonstrated improved outcome scores, quality of life and patient satisfaction, according to data presented at the American Academy of Orthopaedic Surgeons Annual Meeting.
“In the difficult patient population of those with dysplastic hips, arthroscopy has had a controversial role,” said Marc J. Philippon, MD,managing partner of the Steadman Clinic and co-chair and board member of the Steadman Philippon Research Institute. “There is not much evidence to support treatment by arthroscopy in this group. But, a correlation has been shown between hip dysplasia and early-onset osteoarthritis, tears of the labrum and joint failure in the young patient.”
Philippon and his colleagues evaluated data from a prospective data registry to determine survivorship, defined as not requiring total hip replacement, at 3 years to 8 years after hip arthroscopy in patients with dysplastic hips. A single surgeon performed all consecutive hip arthroscopies in the data registry from 2005 to 2011.
Inclusion criteria were primary hip arthroscopy for labral pathology and femoroacetabular impingement with no previous total hip replacement or resurfacing and a center edge angle of 20° or less. Patients were excluded if they were professional athletes or had hip fracture, hips with bone grafting, bone plugs, hemicap implant performed during arthroscopy, underlying hip disease such as Legg-Calve-Perthes, pigmented villonodular synovitis, synovial chondromatosis or labral reconstruction during arthroscopy.
Researchers identified 11 hips that met the inclusion criteria. Patients were an average age of 39 years and the study included six women and five men. Their average centeredge angle was 16°, and their average alpha angle was 69°. All hips had a labral repair, 10 had a femoral neck osteoplasty, and five had a minimal acetabular rim trimming.
Three patients required total hip arthroplasty: a 50-year-old patient at 12 months after the index hip arthroscopy, a 42-year-old patient at 15 months and a 58-year-old patient at 25 months. Two of these patients had a joint space of less than 2 mm.
For those patients who did not require total hip replacement, preoperative modified Harris hip scores improved from 55 points to 74 points postoperatively. The postoperative SF-12 physical component score was 53.2 points and the mean SF-12 mental component score was 53 points. Patients rated their satisfaction at a median of nine out of 10.
“Patients requiring total hip replacement were older and two of the three had limited joint space,” Philippon said during his presentation. “Hip arthroscopy was successful in the younger dysplastic adult with adequate joint space. Patients improved in function and symptoms. They had good general physical and mental health, and high patient satisfaction was reported. We use hip arthroscopy as a first stage in treatment, often to assess the cartilage and the status of the labrum, and we coordinate further treatment in the patient when indicated.” – by Tina DiMarcantonio
References:Philippon MJ. Paper #411. Presented at: American Academy of Orthopaedic Surgeons Annual Meeting; March 11-15, 2014; New Orleans.